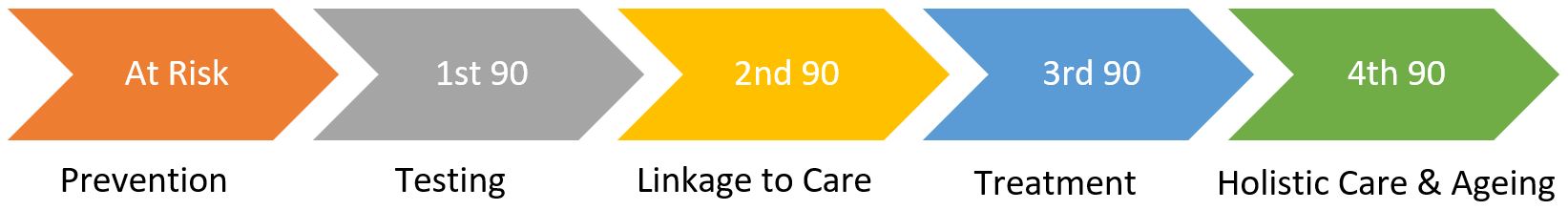
The Human Immunodeficiency Virus (HIV) attacks and destroys CD4 cells, which are part of the immune system. With a weakened immune system, persons living with HIV are more susceptible to other infections and are more likely to develop other complications. HIV treatment is highly effective, allowing persons living with HIV to live long, healthy lives. The CHP follows the steps of HIV care continuum model to provide a variety of comprehensive care to both persons living with HIV and those at risk of HIV infection.
HIV Treatment
Patients who have been diagnosed with HIV and referred to NCID will be given an appointment to consult our physicians within 7 days. After a holistic assessment, patients will start on antiretroviral therapy (ART) to keep the disease under control by reducing the amount of HIV in the body. ART will be initiated as early as possible, with some patients starting on the same day as their first visit (where it is safe and appropriate). After that, patients are seen by their primary physicians regularly to ensure that they respond well to the treatment.
Please click here for more information about our outpatient services.
HIV Co-morbidity Clinics
If required, patients will be referred to doctors from other disciplines to help manage their conditions and minimise the chances of further complications associated with HIV infections. These conditions may include ophthalmology for HIV-related eye conditions, endocrinology for chronic diseases such as diabetes and osteoporosis, psychiatry for mood disorders, and dermatology for HIV-related skin conditions.
Pre-Exposure Prophylaxis (PrEP) Care Clinic
Pre-exposure prophylaxis (PrEP) is a risk-reduction treatment against HIV, which involves the use of ART to prevent HIV transmission. PrEP will be prescribed to HIV-negative individuals who are considered at high risk of acquiring HIV infection. At the initial visit, our PrEP physicians will discuss the eligibility criteria for receiving PrEP, perform HIV/STI testing, and assess kidney function. A PrEP prescription will be issued after that. Patients taking PrEP will also receive sexual health services and counselling.
When taken as prescribed, PrEP is effective in preventing HIV. Since PrEP only protects against HIV, condom use is still important to prevent other sexually transmitted infections (STIs).
If you are considering starting PrEP, please contact the NCID HIV PrEP Clinic at (65) 6357 7000 or email prepcare@ttsh.com.sg. More information about PrEP can be found here.
Post-Exposure Prophylaxis (PEP) Treatment
Post-exposure prophylaxis (PEP) is the use of ART to reduce the risk of HIV transmission following a recent high-risk exposure. It should only be used in an emergency and must be started within 72 hours of a possible HIV exposure. One should consider pre-exposure prophylaxis (PrEP) instead if there is repeated exposure to HIV (see PrEP above).
A high-risk exposure to HIV includes:
any unprotected anal or vaginal sex with multiple sexual partners, or a partner who is HIV positive with an unsuppressed viral load or a person with unknown HIV status,
sharing of or exposure to contaminated needles or blades, particularly needle-stick injuries, or
victims of sexual assault.
Should you require PEP, please visit the TTSH Emergency Department.
Data Management Programme
The Data Management Programme, helmed by a team comprising of a clinician-scientist and data analysts to improve the health and well-being of patients with HIV, serves to monitor and evaluate HIV Clinical Programme services by maintaining a comprehensive clinical database to guide its continuous development and improvement.
The CHP provides holistic allied health services for patients who require specific care. These include care and counselling, HIV specialist pharmacy, inpatient and outpatient nursing, dietetics and nutrition, physiotherapy, occupational therapy and psychological wellness services. If you are a patient seeking care at our centre and have more queries regarding these allied health services, please speak to your physician.
Positive Prevention Programme (PPP)
The PPP offers emotional, social, and financial support to patients and education on safe sexual behaviour. Our MSWs are experienced and specially trained in providing care and support to persons living with HIV. They also assist with spousal notification for newly diagnosed HIV patients.
Defaulter Programme
The Defaulter Programme works closely with physicians and patients to help patients remain engaged in care. HIV care is highly dependent on adherence not only to treatment but also continued engagement with care. The defaulter coordinator plays an essential role in triaging, contacting, and re-engaging with patients who have missed clinic appointments, and in so doing, ensuring that they continue to receive essential care.
Outpatient Nursing
NCID outpatient nurses support NCID's comprehensive HIV care services, which include HIV diagnosis and testing, initial management of newly diagnosed HIV infection, initiation and maintenance of highly active antiretroviral therapy (HAART), and monitoring for long-term HIV complications. They also offer nurse-led vaccinations and immunisations, as well as screening for other chronic diseases.
Inpatient Nursing
NCID inpatient nurses will look after persons living with HIV who require admission for further investigations and treatment throughout their inpatient stay at NCID. They also advocate on behalf of the patients and educate their loved ones about HIV and co-morbidities. Our multidisciplinary HIV care remains seamless from the patient's point of admission to discharge and return to routine outpatient care.
Drug Adherence Programme
The Drug Adherence Programme is led by pharmacists, and aims to prevent HIV treatment failure by providing counselling and care for patients with HIV who have:
recently started on antiretroviral therapy (ART);
changed ART regimen; and/or
experienced difficulties with ART adherence.
Antiretroviral Therapy-Directly Observed Therapy (ART-DOT)
The ART-DOT aims to improve patients' adherence to ART by ensuring that patients who face challenges with ART adherence (as evidenced by persistently unsuppressed viral load) receive their ARTs under the supervision of a pharmacist.
Psychological Wellness Programme
The Psychological Wellness Programme is a service provided by NCID and the Department of Psychological Medicine at TTSH. The programme screens patients for anxiety and depressive symptoms and provides treatment services if needed.
For more information about the Psychological Wellness Programme, please click here.
NCID Cares
NCID's community engagement and outreach arm looks after the medical needs and emotional well-being of patients with HIV/AIDS by providing help through patient rehabilitation and support programmes. Diagnostic test subsidies and financial support to cover medication costs are also provided to needy patients living with HIV. NCID Cares also coordinates volunteer engagement to conduct handicraft workshops, and other volunteer facilitated activities for patients.
For more information on NCID cares, please click here.
The CHP conducts regular training and educational programmes for infectious diseases trainees, healthcare professionals, people living with HIV and the general public to raise HIV awareness and knowledge.
HIV Grand Rounds
HIV Grand Rounds is a regular, structured meeting that discusses standardised HIV care in the local setting. It brings interesting, challenging HIV-based cases for discussion, with the goal of combining learning and edification. The most recent HIV guidelines, local publications influencing practices or policies, and local HIV research findings are shared during this meeting. Clinicians (physicians, trainees, and nurses), pharmacists, medical social workers, laboratory staff, and community partners are all invited to attend the Grand Rounds.
Healthcare Worker HIV Education Series
The Healthcare Worker HIV Education Series is jointly organised by the HIV Programme at National University Hospital (NUH) and NCID. The Education Series is a modular education initiative that runs quarterly. The Education Series aim to improve the HIV knowledge and skills of healthcare workers in Singapore.
Nursing HIV Education Series
The Nursing HIV Education Series is organised by the nursing team at NCID. HIV has progressed from an acute to a highly treatable chronic condition. This series aims to educate nurses and other healthcare workers on the fundamentals of HIV care, such as ART administration, psychological support, and the management of elderly with HIV.
HIV Healthcare Education Posters
The HIV Healthcare Education Posters are designed to educate nurses on the science of undetectable = untransmittable (U=U), avoiding stigmatising people living with HIV, managing needle-stick injuries, and how nurses can support persons living with HIV by connecting them to various support services in Singapore. It aims to empower nurses to embrace science, dispel myths, and be patient advocates.
World AIDS Day (WAD) Event
World AIDS Day started in 1988 and takes place on 1 December each year. It is an international day for people worldwide to unite in the fight against HIV, to show support for people living with HIV, and to commemorate those who have died from an AIDS-related illness. Every year, CHP commemorates WAD through activities to raise awareness about HIV, challenge misconceptions about HIV transmission and infection, and develop empathy and solidarity between people living with HIV and healthcare workers.
For more information on our World AIDS Day events, please click the links below:
2020: We are in this together
2021: Following Jason's Journey: Diagnosis & Beyond