AccordionContent1
AMR
occurs when microorganisms such as bacteria, viruses, fungi and some parasites
develop mechanisms to resist being killed by antimicrobial agents such as
antibiotics. Infections thus persist and may spread to others.
Find
facts on AMR here.
Why is AMR a concern?
AMR
presents a major threat to global health. With the gradual and rising development of resistance to antimicrobial agents, many medicines are increasingly losing their
ability to treat infections. This threatens to reverse the
benefits derived from years of advancements in science and medicine.
WHO warns that drug-resistant diseases could lead to a projected 10 million
deaths globally each year by 20502 and highlights the projected
economic strain from the impact of dealing with prolonged hospitalisation stays
and increased morbidity.
A
study published in the Lancet in 2022 estimated that 4.95 million
global deaths were associated with bacterial AMR in 20193. AMR can
affect anyone, at any stage of life and it is evolving at a
rate that outpaces the development of new antimicrobial agents. With increased
global connectivity through trade and travel, AMR developed in one region has the potential to spread to around the globe.
References:
[1] Antimicrobial Resistance, World Health Organisation, www.who.int
[2] World Health Organisation (WHO) No Time to Wait: Securing the Future from Drug-Resistant Infections. Report to the Secretary General of the United Nations
[3] Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Antimicrobial Resistance Collaborators. Lancet 2022; https://doi.org/10.1016/ S0140-6736(21)02724-0
AccordionContent2
Judicious
prescribing of antimicrobials plays a key role in minimising the risk of
misuse. Ensure the 4 Rights when prescribing, dispensing or administering
antimicrobials to patients: Time, Dose, Duration and Antimicrobial Agent.
Healthcare professionals should prioritise educating their patients on
the importance of appropriate antimicrobial use, to receive the recommended
vaccines, and maintain good hygiene habits to prevent the spread of infections.
Appropriate
infection prevention and control measures will further reduce the
spread of antimicrobial-resistant organisms. Healthcare professionals should also stay equipped
with updated knowledge and keep abreast of resistance patterns in their institutions and the community to improve antimicrobial use in clinical
practice. Lastly, supporting institutional and national AMR surveillance
programmes, and promptly reporting any AMR outbreaks to the appropriate
authority are actions essential to control the spread of AMR.
Download AMR material to display at your institution:
Infection Control
Guidelines for Healthcare Facilities can be found here.
AccordionContent3
In May
2015, the World Health Assembly endorsed a Global Action Plan that sets out key
priority areas to combat AMR, including improving AMR awareness, optimising the use of antimicrobials, strengthening
surveillance and research, and reducing infections. Singapore's National Strategic Action Plan (NSAP) on AMR was launched in 2017 and is aligned with these global objectives.1
Read
more about the WHO Global Action Plan on AMR here.
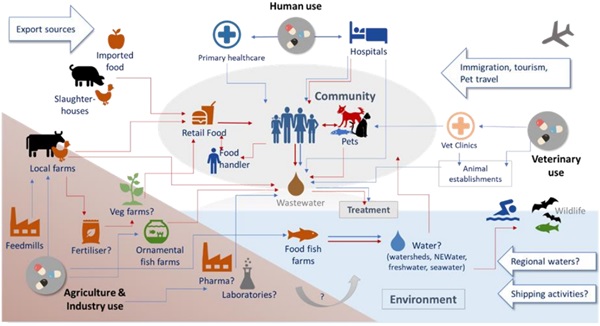
A 'One Health' approach in combating AMR through
cross-sectoral collaboration is essential and
is highlighted in Singapore's National
Strategic Action Plan (NSAP) on AMR. The NSAP brings together the Ministry of Health (MOH), Health Promotion Board (HPB), National Parks Board
(NParks), National Environment Agency (NEA), Singapore Food Agency (SFA), and
PUB, Singapore's National Water Agency, to coordinate and drive AMR efforts
across the human, environmental, food and animal sectors through a multi-agency national workgroup. The NSAP aims to reduce the emergence and prevent the spread of drug-resistant organisms through five core strategies:
Raising awareness and understanding of AMR and appropriate antimicrobial use through Education.
Understanding the levels, distributions and trends of resistant organisms and antimicrobial use through regular Surveillance and Risk Assesment.
Filling in gaps in knowledge and improving our understanding of the AMR situation through Research.
Reducing the spread of drug-resistant organisms through effective Prevention and Control of Infections.
Reducing inappropriate antimicrobial use and preserving the effectiveness of medicines through the Optimisation of Antimicrobial Use.
References:
[1] National Strategic Action Plan (NSAP) on Antimicrobial Resistance, Singapore
AccordionContent4
In
September 2018, the Antimicrobial
Resistance Coordinating Office (AMRCO) was established to drive the implementation and
monitoring of the NSAP, coordinate AMR efforts across different sectors and
serve as secretariat for national AMR committees.
Learn
more about AMR efforts undertaken by AMRCO in education, surveillance and risk
assessment, research and optimisation of antimicrobial use in the subsequent
sections.
AccordionContent5
Public education is a cornerstone in the fight against AMR. Raising awareness and understanding of AMR will prevent the misuse and overuse of antimicrobials and help to reduce the spread of infections. Coupled with professional education and training for healthcare professionals, this will lead to impacts on the sustainable and responsible use of antimicrobials at the individual as well as societal level.
World AMR Awareness Week social media campaigns
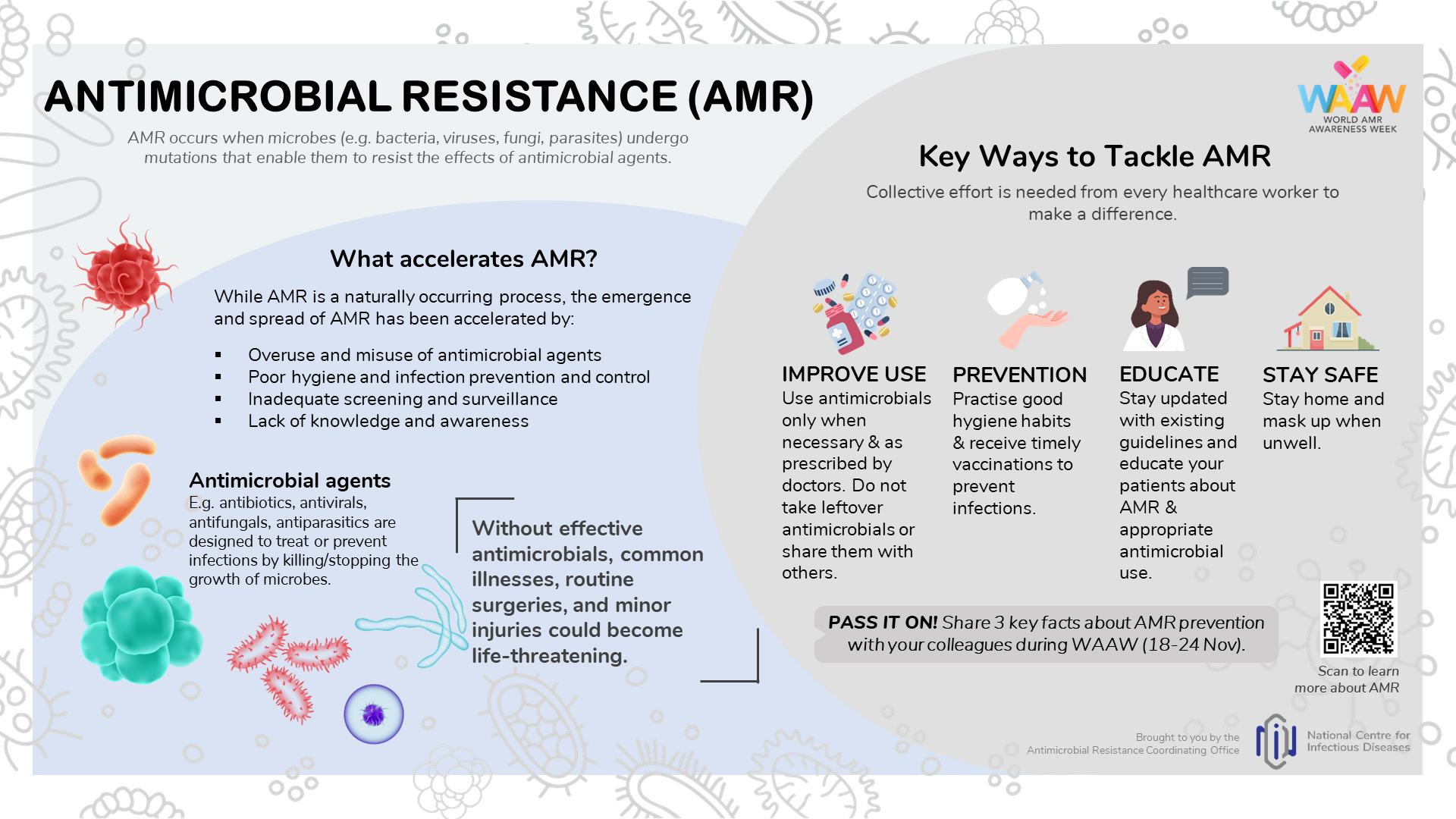
Held annually from 18 to 24 November, the World AMR Awareness Week (WAAW) aims to increase awareness of AMR and encourage best practices among the public, healthcare workers and policy makers to prevent further emergence and spread of AMR.
During WAAW, AMRCO regularly runs a campaign on NCID's social media channels to highlight AMR as a global public health concern, what the public can do to play their part, and why the One Health approach matters.
Download these AMR graphics for sharing on social media:
2022 Campaign
2023 Campaign
Sharing of winning entries from the AMR Competition 2023
Professional training for healthcare professionals
Healthcare professionals are kept up to date on AMR issues and appropriate prescribing of antimicrobials through continuing professional education events.
For upcoming training events, click here.
Past AMR training events include:
- Primary Care Forum 2019 and 2020
- Continuing Nursing Education Webinar on AMR 2021
- WAAW Inter-hospital Webinar Series (held in collaboration with Singapore's private and public hospitals)
AccordionContent6
Surveillance of AMR and antimicrobial utilisation is essential to understand the magnitude, distribution and impact of resistant organisms and antimicrobial use. Regular monitoring of resistance trends, associations between usage and resistance, and outcomes of policies and initiatives to combat AMR will help enable a timely and appropriate response to AMR.
One Health surveillance report on antimicrobial utilisation and resistance

| The two-yearly One Health Report on Antimicrobial Utilisation and Resistance is a collaboration between MOH, NEA, NParks, PUB, SFA and AMRCO, NCID. The multi-sectoral surveillance report provides an overview of national surveillance programmes and presents key findings on antimicrobial utilisation and resistant organisms in the human, animal, food and environmental sectors in Singapore. Programmes include surveillance on the utilisation and sales of antimicrobials in the human and animal health sectors, incidence and resistance proportions (%R) of priority AMR organisms found in humans, animals, food and the environment. More information can be found in the reports below: One Health Report on Antimicrobial Utilisation and Resistance, 2017 One Health Report on Antimicrobial Utilisation and Resistance, 2019 One Health Report on Antimicrobial Utilisation and Resistance, 2021 |
Primary Care Antimicrobial Utilisation Surveillance InitiativeThe Primary Care Antimicrobial Utilisation Surveillance Initiative (GP-AMU) which was launched in 2021, monitors antimicrobial utilisation (AMU) trends in the community through analysing and reviewing AMU data contributed by participating general practitioner (GP) clinics. In turn, GP-AMU facilitates data-driven feedback on an annual basis for participating GP clinics' internal monitoring. Learn more about GP-AMU here.
If you are interested to participate in this initiative, please contact [email protected] for more information.
Contributing AMR data to WHO GLASS
In 2019, Singapore enrolled in the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS), the first global collaborative effort to standardise AMR surveillance. Singapore has been contributing AMR data from sentinel healthcare facilities through the AMRCO, which is the appointed GLASS National Coordinating Centre.
Learn more about WHO GLASS here.
The GLASS dashboard presents global AMR data for countries, territories, and areas (CTAs) that are enrolled in GLASS. View the GLASS dashboard here.
AccordionContent7
Research helps to fill gaps in knowledge, improve our understanding of the AMR situation and enhance tools and measures needed to help control this complex problem. AMRCO serves as the national body to coordinate One Health AMR research across the human, animal, food and environment sectors, and the funding of One Health AMR research.
One Health AMR Research Programme
The One Health Antimicrobial Resistance Research Programme (OHARP) is jointly funded by MOH, NEA, NParks, PUB, and SFA. NCID is the appointed grant intermediary which provides grant administration and management support for OHARP grants.
OHARP supports One Health AMR research in the following research priority areas - Knowledge, Attitudes and Practices (KAP); Transmission Pathways; and Socioeconomic Impact of AMR.
For more information on OHARP, please click here.
One Health AMR Research in Singapore
 | In addition to improving our understanding of resistance development, it is also necessary to be informed of where the gaps in evidence lie so that resources for research could be allocated appropriately. AMRCO regularly conducts the review of the AMR research landscape in Singapore to understand the current research trends and topics in AMR, as well as the AMR research expertise in Singapore. The ongoing review will also identify opportunities for research, with the goal of fostering collaborations among scientists from different domains, especially across sectors, to develop novel tools, strategies and methods to address AMR. The first comprehensive review of AMR research articles published by Singapore's research community from 2009 to 2019 has been completed. Findings derived from the review provided important insights will guide us in prioritising One Health AMR research efforts. The charts below show information on the trends of AMR research published:
|
(A) Overall annual publication trend, 2009-2019
| (B) Annual publication trend by research domain, 2009-2019
.png) |
(C) Overall distribution of research publication by research domains .png)
| (D) Distribution of research publications by the One Health sectors
.png)
|
(E) Annual publication trend by the One Health sectors
.png)
| (F) Distribution of institutional research output of research domain
.png)
|
Please refer to the report for more information on AMR research trends in Singapore, and the recommended areas of research across sectors.
AccordionContent8
Inappropriate use of antimicrobials is the largest driver of AMR. Infections with organisms resistant against last-line antimicrobials have already been observed in patients in Singapore. Measures must therefore be taken to conserve existing antimicrobials. The implementation of antimicrobial stewardship programmes promotes rational prescribing practices, slows the emergence of resistance and reduces risks to the healthcare system.
Antimicrobial stewardship programme
Antimicrobial stewardship programmes (ASP) have been implemented in all public hospitals since 2011. This includes the establishment of ASP teams consisting of infectious diseases physicians and pharmacists. The tracking of antimicrobial usage, appropriateness of antimicrobial use and ASP intervention acceptance rates are reported regularly to hospital management and ASP teams.
The Infectious Diseases Research and Training Office holds the Singapore Antimicrobial Stewardship Training Course annually with the aim of empowering individuals with the knowledge and skills needed to establish and operationalise effective ASPs. Follow this link to the NCID events page for details of the latest events.
National surgical antibiotic prophylaxis guideline (Singapore)
.jpg)
| The National Surgical Antibiotic Prophylaxis (SAP) Guideline (Singapore) provides evidence-based recommendations for the rational use of antibiotic prophylaxis, including recommended agent(s), dose, timing and duration for adult patients undergoing clean or clean-contaminated surgeries. This guideline aims to align best practices nationally and provide a framework for audit and surveillance. The establishment of the national SAP guideline for hospitals in Singapore may reduce the rate of surgical site infections, while also reducing adverse events from prolonged duration of surgical prophylaxis.
The guideline was developed through a multidisciplinary collaborative effort by the National Antimicrobial Stewardship Expert Panel (NASEP) National SAP Guideline Development Workgroup, comprising Infectious Disease (ID) physicians, ID and/or antimicrobial stewardship-trained pharmacists, surgeons, and anaesthesiologists; and endorsed by NCID and the Chapter of ID Physicians, College of Physicians, College of Anaesthesiologists and College of Surgeons under the Academy of Medicine, Singapore. Download a copy here.
|
AccordionContent9
AccordionContent10
AccordionContent11
AccordionContent12